Selective Enoxaparin Protocol Reduces Wound Hematomas Without Raising Postpartum VTE Risks: JAMA
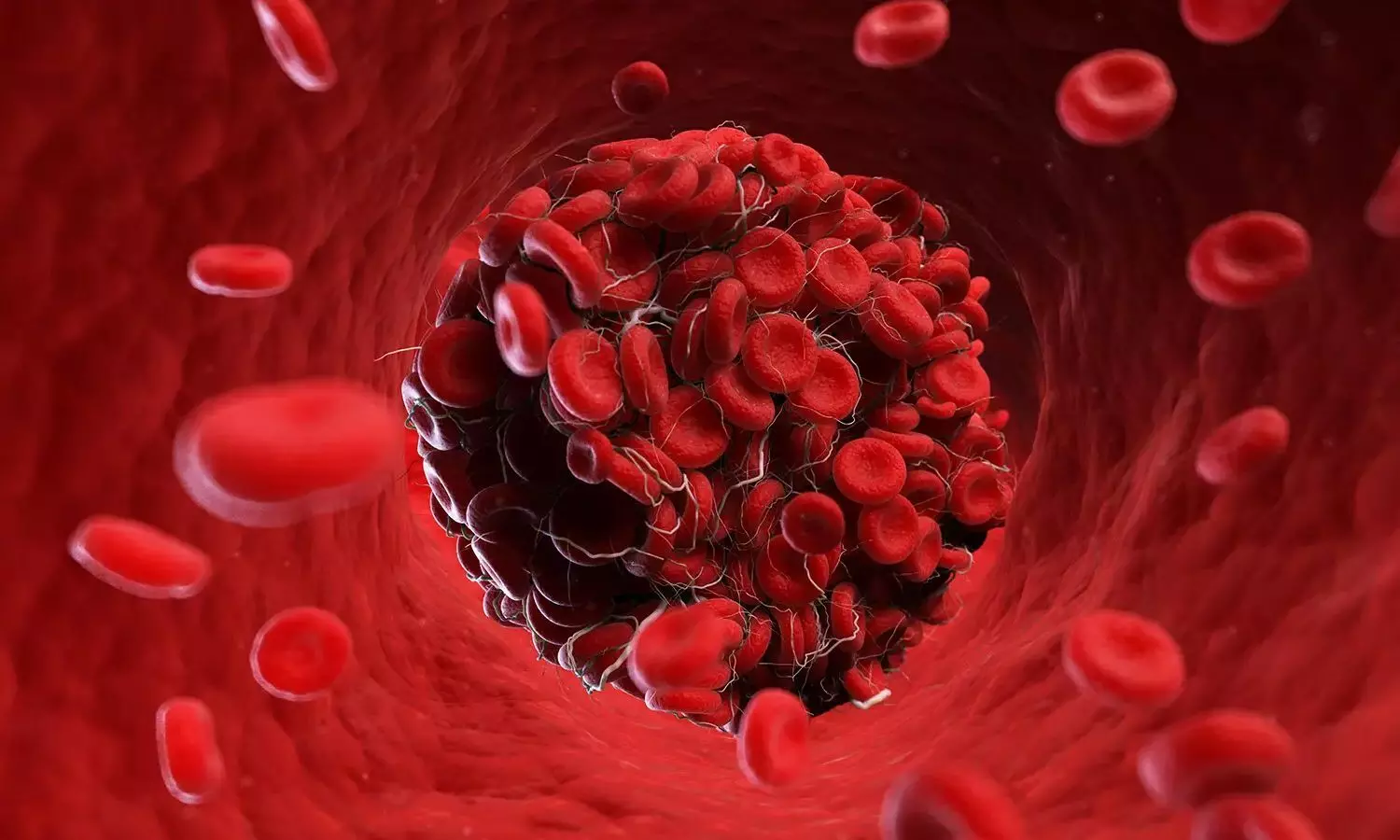
USA: The approach to thromboprophylaxis—preventing blood clot formation—has long been a critical consideration in obstetric care due to the increased risk expectant mothers face.
A recent study has demonstrated two strategies: the traditional standard risk-stratified heparin-based protocol versus a newer, more selective approach. Both techniques mitigate the risk of venous thromboembolism (VTE), a potentially life-threatening complication during pregnancy and the postpartum period.
The retrospective observational study, published in JAMA, found that a more selective protocol for postpartum enoxaparin was associated with reduced rates of wound hematomas without evidence of increased rates of postpartum thromboembolic events.
A more selective protocol for chemoprophylaxis led to a decrease in heparin (enoxaparin) administration (16% versus 8%), the researchers reported. The selective protocol for postpartum enoxaparin was associated with a reduction in wound hematoma (0.7% versus 0.3% in the selective protocol group; adjusted odds ratio, 0.38) without evidence of a rise in VTE (0.1% versus 0.1% in the selective protocol group; adjusted odds ratio, 0.40).
In 2016, a pregnancy-related VTE prophylaxis protocol was adopted based on American College of Obstetricians and Gynecologists guidelines that recommended postpartum heparin-based chemoprophylaxis (enoxaparin) based on a risk-stratified algorithm.
In 2021, a more selective risk-stratified approach was implemented in response to higher occurrences of wound hematomas, despite no significant decrease in VTE with the existing protocol. In the study, Macie L. Champion, St David’s Medical Center, Austin, Texas, and colleagues aimed to evaluate outcomes of the more selective risk-stratified approach to heparin-based obstetric thromboprophylaxis (enoxaparin) protocol.
The retrospective observational study included 17,489 patients who gave birth at a single tertiary care center in the southeast US. Data collection was between 2016 and 2018 for the original protocol period, and between December 1, 2021, and May 31, 2023, for the more selective protocol period. Patients receiving outpatient anticoagulation for active VTE or deemed at high VTE risk during pregnancy were excluded from the study.
The study compared outcomes between two postpartum VTE chemoprophylaxis protocols: the standard risk-stratified protocol and the more selective protocol. The primary outcome measured was the clinical diagnosis of wound hematoma within six weeks after childbirth. Secondary outcomes included new diagnoses of VTE within the same postpartum period. Researchers analyzed baseline characteristics and outcomes across both protocol groups and calculated adjusted odds ratios with 95% confidence intervals, using the original protocol group as the reference point for comparison.
The study led to the following findings:
- Of 17 489 patients included in the analysis, 71% were in the original protocol group, and 29% were in the more selective group.
- Rates of chemoprophylaxis decreased from 16% (original protocol) to 8% (more selective protocol).
- Patients in the more selective group were more likely to be older, be married, and have obesity or other comorbidities (hypertension, diabetes, cardiac disease).
- Compared with the original protocol, the more selective protocol was associated with a decrease in any wound hematoma (0.7% vs 0.3%; adjusted odds ratio [aOR], 0.38), specifically due to a lower rate of superficial wound hematomas (0.6% versus 0.3%).
- There was no significant increase in VTE or individual types of VTE (0.1% versus 0.1%; aOR, 0.40).
"Our findings showed that implementing a more selective risk-stratified approach in an enoxaparin thromboprophylaxis protocol for venous thromboembolism was linked to lower rates of wound hematomas, without a corresponding increase in postpartum VTE rates," the researchers concluded.
Reference:
Champion ML, Blanchard CT, Lu MY, et al. A More Selective vs a Standard Risk-Stratified, Heparin-Based, Obstetric Thromboprophylaxis Protocol. JAMA. 2024;332(4):310–317. doi:10.1001/jama.2024.8684
from Medical News, Health News Latest, Medical News Today - Medical Dialogues | https://ift.tt/QsmwFVe
Comments
Post a Comment