Total Blastocyst Usable Rate: A New Independent Predictor of Cumulative Live Birth Rate in IVF Cycles, study reveals
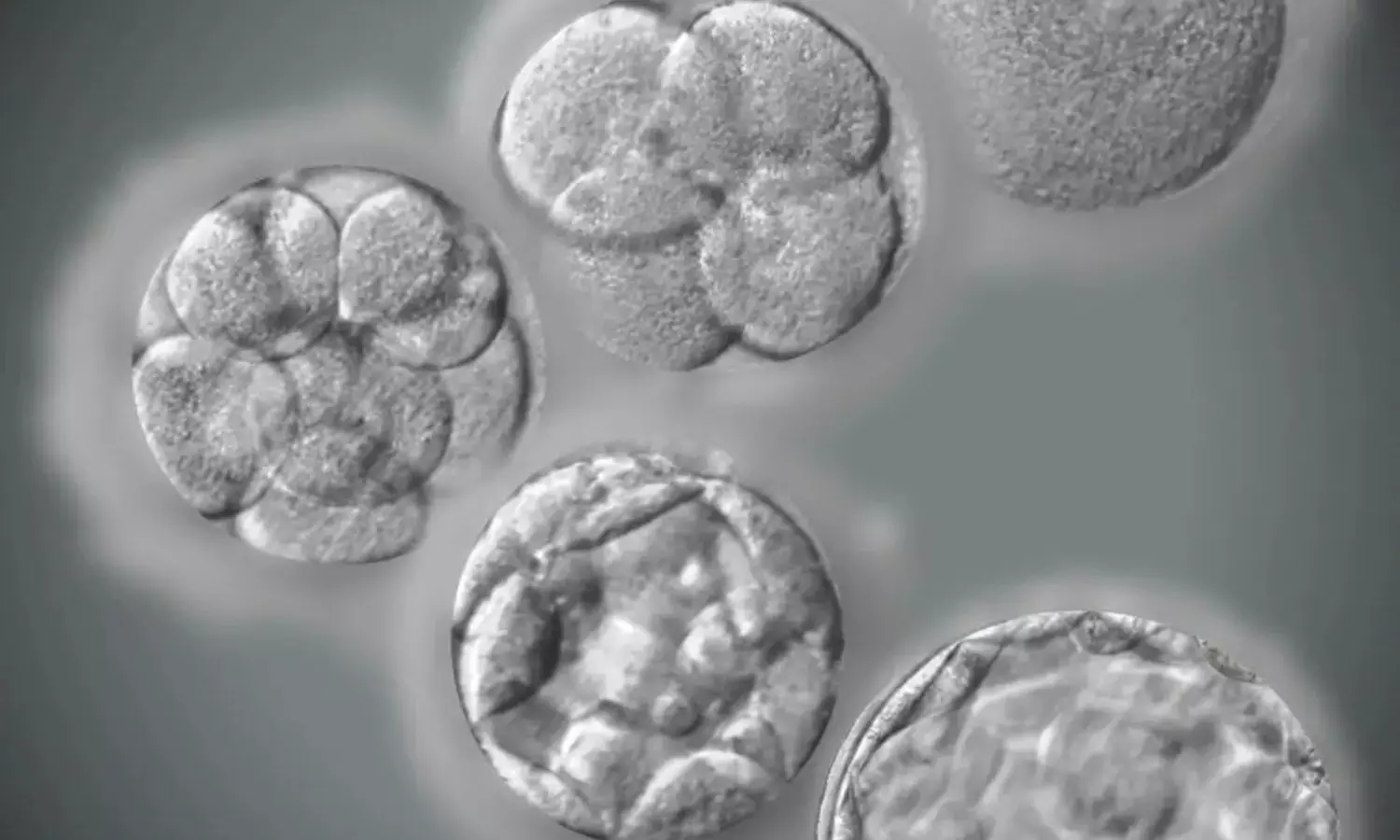
France: In a groundbreaking development for assisted reproductive technology, researchers have identified a pivotal predictor of success in in vitro fertilization (IVF) cycles: the Total Blastocyst Usable Rate (TBUR). This newly recognized metric has emerged as a significant indicator of the cumulative live birth rate following IVF procedures, potentially revolutionizing how fertility clinics approach treatment strategies.
In the study published in the Journal of Gynecology Obstetrics and Human Reproduction, the researchers reported for the first time that TBUR is independently and positively associated with the cumulative live birth rate (CLBR) in IVF cycles.
The findings suggest that the total blastocyst usable rate reflects the overall quality of the embryonic cohort.
"Our results illustrate that TBUR is a valuable prognostic factor of cumulative live birth rate in IVF cycles, which might serve as a tool for lab monitoring, cycle analysis by medical staff, and patients’ counseling," the researchers wrote.
Despite advances in IVF techniques, it is crucial to determine the prognostic factors influencing CLBR for optimizing outcomes. Among several key performance indicators in the lab, blastulation rate, and more precisely, the total blastocyst usable rate, has gained particular interest. In the study, Thomas Freour, Department of Biology and Reproductive Medicine, University Hospital of Nantes in Nantes, France, and colleagues aimed to determine if TBUR was significantly associated with CLBR.
For this purpose, they conducted a monocentric retrospective case-control study in 317 consecutive IVF/ICSI cycles in 2014–2020, which led to the formation of three usable blastocysts, including freeze-all cycles.
The study assessed TBUR, calculated as the ratio of usable blastocysts to 2PNs (pronuclei), and recorded CLBR after a two-year follow-up period, incorporating fresh and frozen embryo transfers. CLBR outcomes were compared between two distinct groups based on TBUR: Group 1, characterized by TBUR ≥50%, and Group 2, with TBUR ≤30%.
The key findings of the study were as follows:
- CLBR was significantly higher in group 1 than in group 2 (57 versus 41 %).
- Adjusted logistic regression showed a statistically significant relationship between CLBR and TBUR, with a significantly lower chance of achieving a live birth in group 2 than in group 1 (OR = 0.408).
While the study's single-center approach and the subjective selection of TBUR thresholds and blastocyst numbers warrant careful consideration before applying the findings broadly, the results demonstrate that TBUR serves as a significant predictive factor for CLBR in IVF cycles. This finding suggests its potential utility for laboratory monitoring, cycle analysis by healthcare professionals, and patient counseling.
"These findings align with the principles of P4 medicine (Predictive, Preventive, Personalized, and Participatory) and underscore the need for continued research to enhance embryo culture conditions," the researchers concluded.
Reference:
Chaillot, M., Reignier, A., & Fréour, T. (2024). Total blastocyst usable rate is a predictor of cumulative live birth rate in IVF cycles. Journal of Gynecology Obstetrics and Human Reproduction, 53(8), 102809. https://ift.tt/0dUxabV
from Medical News, Health News Latest, Medical News Today - Medical Dialogues | https://ift.tt/USLpOo3
Comments
Post a Comment